Is a thyroidectomy scar a permanent reminder of a necessary procedure, or can its visibility be effectively managed? The truth is, while a scar is almost inevitable with traditional thyroidectomy, its appearance and impact can be significantly minimized through proactive care and informed choices.
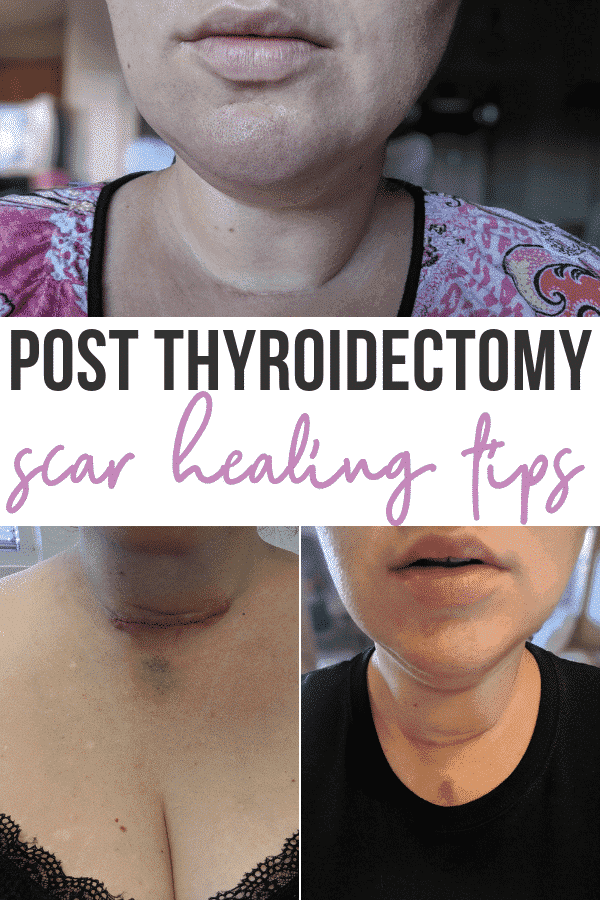
Traditional thyroidectomy, a surgical procedure commonly performed at leading medical institutions, typically leaves a scar on the anterior neck. This scar, usually ranging from 1 to 2 inches in length, is carefully positioned within a skin crease. The strategic placement of the incision is a deliberate effort to promote optimal healing and, importantly, minimize its visibility. The aim is not just to ensure the surgery's success but also to address the patient's cosmetic concerns by making the resulting scar as inconspicuous as possible.
The management of a thyroidectomy scar involves multiple facets, each playing a crucial role in the final outcome. One of the most effective forms of scar therapy involves the use of silicone rubber. Silicone products are known to aid in the flattening of raised, or hypertrophic, scars and to reduce their redness, a characteristic that distinguishes them from surrounding skin. While the precise mechanisms by which silicone improves scar appearance are not fully understood, numerous studies have demonstrated its efficacy.
Post-surgery care is paramount for achieving the best possible outcome. A cornerstone of scar management is gentle but firm massage. Approximately two weeks after the surgery, patients are typically advised to massage the scar for about five minutes, several times a day. Vitamin E oil is often recommended for this purpose, as it can aid in moisturizing the area and promoting healing.
Many patients grapple with the question of how best to address the appearance of their thyroidectomy scar. This leads to two distinct schools of thought: some prefer to cover the scar, while others choose to embrace it as a visible symbol of their journey. There is no right or wrong answer, as the decision is profoundly personal and dependent on individual comfort and aesthetic preferences. Various options exist for covering the scar, including scarves and other forms of clothing, offering flexibility and accommodating different lifestyles.
Certain individuals may be predisposed to more significant scarring. For those with a history of keloids, which involve excessive scar tissue formation, the risk of experiencing more pronounced scarring after thyroid surgery is increased. However, the location of the incision on the neck actually minimizes the likelihood of keloids, due to the unique properties of the skin in that area. People with darker skin tones may also find their scars more noticeable due to the contrasting color between the scar tissue's pigmentation and the surrounding skin color.
It's imperative for patients to recognize and report any unusual symptoms. If you observe any signs of excessive or atypical scarring, it is advisable to promptly inform your physician. Timely intervention can potentially prevent or mitigate complications and help ensure the best possible aesthetic outcome.
Scar size is a significant factor in the overall appearance. Surgeons take great care to minimize the incision's size and strategically place it within natural skin creases. These measures are taken to reduce the scar's visibility on the neck. The goal is to create a scar that, over time, fades into a thin line, though in some instances, scars may become more noticeably thickened. This variability underscores the importance of personalized care and ongoing assessment.
The primary goals of therapy in the postoperative period are to modulate the scar's development early on in order to reduce the likelihood of it thickening. This involves a rigorous approach, starting with gentle massage, and may include the use of silicone products or other treatments. Early intervention and consistent care are critical in shaping the scar's appearance.
For those who are already dealing with a noticeable scar, thyroidectomy scar revision presents a valuable option. This procedure can help reduce the prominence of the scar, blending it more harmoniously with the surrounding skin. Beyond aesthetic improvements, scar revision can address any neck asymmetry or tissue changes resulting from the surgical procedure. Tissue reshaping or augmentation techniques may be incorporated to achieve the desired results and enhance the patient's overall satisfaction.
Advancements in surgical techniques have led to the development of minimally invasive thyroid surgery. This approach is primarily characterized by a reduced incision length, which translates to several key benefits. Patients undergoing this type of surgery often experience less postoperative pain, a shorter hospital stay, and, most importantly, improved cosmetic results. These minimally invasive techniques, introduced within the past 15 years, represent a significant step forward in the surgical management of thyroid disease, aiming to achieve outcomes with minimal patient discomfort and complications.
A specific type of minimally invasive surgery, known as transoral thyroidectomy, provides another avenue for minimizing scarring. This procedure involves the removal of the thyroid gland through the mouth, thereby eliminating the need for an external incision and leaving no visible scar. This innovative approach is an option for certain patients and represents a significant advance in the field of thyroid surgery.
The appearance of a thyroidectomy scar can be a source of understandable concern for patients. To address these concerns, surgeons often provide thorough guidance on scar management and potential treatment options. Regular follow-up appointments are crucial to assess the scar's progress and identify any emerging issues.
The journey of scar healing takes time, with noticeable improvements often occurring gradually. While scars often appear more prominent in the initial stages of healing, they tend to fade and become less noticeable over time. It may take up to 12 months for a scar to reach its final stage, emphasizing the importance of patience and consistent care throughout the healing process.
The cosmetic outcome of the scar after thyroidectomy has raised wide interest in thyroid surgeons, and many attempts to minimize thyroidectomy scars have been performed. Following the recommendations provided by medical professionals does not guarantee that the incision will be imperceptible and/or not produce a noticeable scar.
Thyroid surgery is frequently performed to treat thyroid cancer or thyroid nodules. It is also occasionally used to address hyperthyroidism, although this is less common. The surgery typically involves the removal of part or all of the thyroid gland and is generally considered safe and effective. It is important to consider that there is not a guarantee that the incision will be imperceptible and/or not produce a noticeable scar, and the outcomes may vary from person to person.
The process of wound care is a critical element. Proper wound care, including keeping the incision clean and shielding it from sun exposure, can further improve healing and reduce the appearance of scars. The use of a high SPF sunscreen, such as SPF 30, or covering the scar with a scarf for an entire year, is often recommended. Protecting the scar from the sun's harmful rays provides the best cosmetic outcome for the neck wound. It is crucial to ensure that the wound is fully healed before applying sunscreen.
In conclusion, minimizing scarring after thyroid surgery demands a multifaceted approach that combines proper wound care, specialized scar management techniques, and guidance from a healthcare professional. This holistic approach helps to optimize the healing process and reduce the prominence of any resulting scars.
| Category | Details |
|---|---|
| Procedure Name | Thyroidectomy |
| Purpose | Treat thyroid cancer, thyroid nodules, or hyperthyroidism. |
| Common Incision Location | Anterior neck, often within a skin crease. |
| Typical Scar Length | 1 to 2 inches |
| Scar Management Techniques | Silicone products, scar massage (e.g., with vitamin E oil), scar revision, sunscreen, scar coverings. |
| Healing Time | Scars take up to 12 months to reach their final stage. |
| Minimally Invasive Options | Reduced incision length, Transoral thyroidectomy (scarless) |
| Important Considerations | Sun protection, proper wound care, consultation with surgeon, individual skin type, history of keloids, and prompt reporting of unusual symptoms. |
| Reference | The American Thyroid Association |